The GLP-1 discourse needs a little more nuance
Progress is unequal, and sometimes it has trade-offs. We should talk about them more.
This is not a post arguing against GLP-1 agonist drugs in any way.
GLP-1s are a miracle drug. In 2023, the US obesity rate fell for the first time in decades — from 41.9% in 2020 to 40.3%.1 That’s 4.2 million fewer obese Americans, likely, at least in a part, a result of the more widespread adoption of drugs like Ozempic, Mounjaro, and Zepbound.
The miracle — I’m sure you’re aware — only begins at obesity. Increasing research shows GLP-1s are effective against many chronic diseases that are downstream of excess weight: stroke, heart disease, and kidney disease to name a few. Whether those effects are entirely attributable to weight reductions isn’t yet clear, but the likely answer is: there’s more going on.
They also appear to treat, probably by dampening the brain’s reward system, drug addiction and alcoholism. And new studies are coming out all the time highlighting the drugs’ efficacy across a wider range of conditions. One from November of this year showed GLP-1s reduced knee arthritis pain in overweight adults — and that effect appeared to be independent of weight loss, probably because of reductions in inflammation.
So: It is not a stretch to say we shouldn’t even refer to these as “weight loss drugs,” at least exclusively. And I would not be surprised if, as more people get on them, we continue to see surprising byproduct effects, especially via reduction of compulsive behavior pathways, on things that aren’t even in the conversation: doomscrolling, workaholism, etc. etc.
More to the point: As GLP-1s become more common, I think it’s likely that premature deaths from a variety of causes begin to decrease in the US — possibly even in the next few years, definitely in the medium-term.
And they will become more common. The Biden administration recently proposed covering GLP-1s for people with cardiovascular disease on Medicare. That’s good. They should expand it to obesity too — although there needs to be a federal approval to remove Medicare’s restriction on anti-obesity drugs for coverage to be even wider, and ideally they’d do that before RFK takes the helm.
This is, let’s be clear, a monumental public health victory. GLP-1s should be offered as first line treatment option for anyone with obesity — and probably for other conditions too. They should be cheaper. They should be widely accessible. They should be celebrated.
And they are, all the time, on my feed.
But I sometimes think my timeline is too progress-pilled, too techno-optimist to acknowledge the unsettling fact that the current state of the art treatment for obesity is:
a drug that acts on the brain
costs a lot of money
has to be taken for life
likely to have hugely inequitable distribution for the foreseeable future
and does not work for everyone
My argument is not that we need to course correct.
My argument is that the discourse needs a little more nuance, because:
GLP-1 supply is not going to meet demand for years, and possibly for a decade or more. Even when it does, there will still be tens of millions of Americans — and hundreds of millions of people around the world — who either do not respond or cannot tolerate GLP-1s. We need to do a better job of considering them now.
That we haven’t figured out a better solution to the obesity epidemic is sad, reflects our near-total inability to control diet-related negative externalities on people’s health. It needs to be acknowledged for what it is: a little dystopian. To be clear: we don’t really have other options that work.2 But I think it’s worth lingering on why coordination on this problem is so hard because right now we’re at risk of polarizing it.
More to the point: we aren’t fully aware of the trade-offs we’re making. Yes, we have long-term data on GLP-1s and diabetes — they appear relatively safe. But I don’t see enough people considering even the small possibility that having a huge portion of the population on GLP-1 drugs long-term, may have unintended consequences — if not for them, almost certainly for society, and maybe in weird and unpredictable ways. Some of these, for instance plummeting ultra-processed food sales, might be good. But I want to seriously consider that while this is a cheap lunch, it is not a free lunch.
Supply
GLP-1s are miracles — for 80% of the population
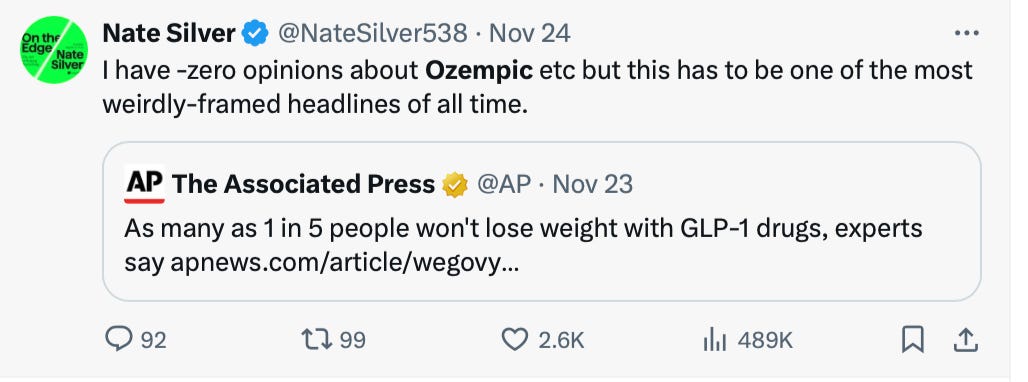
Last week, everyone seemed to jump on the AP for this headline:
Yea, the media is negative. But I feel fine taking the contrarian bait here: 1 out of 5 is a lot!
We’ve been talking, often breathlessly, about the efficacy of GLP-1s for over a year. Emerging research from real-world settings suggests that our expectations of weight loss in real-world settings should be titrated compared to early clinical trials. A September JAMA article for instance found when prescribed for weight loss the mean weight reduction for both semaglutide and liraglutide in one year was -5.9%.3 Tirzepatide and other pipeline treatments may be more effective, but I would expect the overall trend of lower real-world effectiveness to stand.
As a corrective to the media frenzy of the past year, and as a way to dampen expectations that might actually need to be dampened, I think the headline is…fine?
GLP-1s don’t work for everyone for two different reasons:
Somewhere between 10-15% of people are non-responders. Some people have genetic variations in their GLP-1 receptors that affect how well they bind to the medication. Some people develop compensatory mechanisms and don’t actually eat much less. For whatever reason, some people do not lose weight.
GLP-1s have low adherence rates. While some of this is an artifact of inconsistent supply, it is mostly due to side-effects. The most severe, medically, are inflammation in the pancreas, paralysis of the stomach muscles, and bowel obstructions. But many people also report nausea so bad they discontinue, extremely low energy levels, extreme muscle loss, and other degradations in quality of life that are — I’d like to emphasize — so severe they are, by revealed preference, worse than obesity.
Many side effects do appear to abate over time. However, since the first people to get them are likely to be the those who are also more skilled at managing them, we might expect the trends on this to get worse, not better. The good news here is that we are learning more and more about why GLP-1s lead to side-effects, and in the future may be to develop even more targeted treatments. It is far more common to hear people describe these drugs as life-changing, and I don’t want to short-change that.
But you don’t have to dig far to find examples of people who describe their experience as hell. If I can correct anything, it is the underlying optimistic assumption that GLP-1s are a win-win-win. For the most part, I think the quality of life of being a normal weight far outweighs even any long-term side effects. But that isn’t true of everyone.
All this, of course, assumes people can access them.
Supply is constrained
The best piece of media I’ve consumed related to GLP-1s is Acquired’s history of Novo Nordisk. It was the first inkling I had of how wide-reaching they might be — the line they used was “miracle drug for humanity,” and I think that isn’t an exaggeration.
But when the podcast talked a lot about supply constraints, I realized we had no solid numbers. So I reached out to Greg Justice, a forecaster with Samotsvety, to understand just how constrained we were.
What became his Asterisk piece landed on I think a surprising and under-discussed number. By 2030, we’re likely to have sufficient GLP-1 supply for just 23 million Americans — about 4x as many are now taking it, but still far, far short of the 100 million obese people — to say nothing of overweight —- who might benefit.
Greg’s estimate could very well be off. For one, he didn’t factor compounding into his estimates — at the time it was unclear how widespread this was happening, whereas now even Hims is selling compounded semaglutide. Still, I have yet to see any convincing arguments to the contrary. Even if we assume supply is double Greg’s projection, we’re facing supply constraints for the foreseeable future.
After 2030, I’m not sure what to think, and much of that will depend on how strong demand remains over the next five years, a function of, among other things, insurance approvals, further research, discontinuation rates, and a bunch of things that fall under the nebulous bucket of “culture.” But it remains more likely than not in medium-term, millions of people who might benefit from GLP-1s will be unable to get them.
I’m worried here, one, about stigma. We are already in a place where obese people are deeply shamed for a perceived lack of self-control. It seems a likely possibility that this stigma grows over time. We should have a little more empathy for people who have tried GLP-1s and bounced off.
What I’m more worried about is that in the enthusiasm to embrace GLP-1s, we’ve over-corrected into not caring enough about the upstream determinants of why people become obese in the first place. The right seems to be in-fighting about this right now, and I think it’s worth considering why.
New worlds
Imagine a world where we created an anti-depressant/anti-anxiolytic that was vastly superior to SSRIs, NDRIs, MAOIs, etc. It’s good for work productivity. In low doses it can calm your nerves. In moderate doses it affects euphoria. People take it before parties. In fact, if you want to trip with it in high doses, you can. Doctors prescribe it freely, insurance covers it without question, supervisors encourage it for workplace use. There are no side effects. It’s almost entirely free of stigma — people talk about their doses at dinner parties. The government, in fact, subtly encourages its use. It is basically a win-win-win-win.
This is of course the plot of Brave New World. That people find GLP-1s a little dystopian, that they push back, shouldn’t be surprising. If Ozempic appeared in a book 50 years ago, it would be a dystopian novel, and it would have been lambasted for ripping off Huxley. Its theme would be that there is something rotten with the system and culture that is so eager to embrace techno-fixes as it turns its eyes away from the root cause — however complex — of its problems.
GLP-1s aren’t a perfect analogy to soma. Under any sane cost-benefit analysis, GLP-1s come out extremely positive. But there are costs, even if those costs are difficult to quantify. And one of those is that we’re even less likely now to figure out the coordination problems that have led to the obesity epidemic in the first place.
I spent a chunk of my PhD research various forms of regulation of the food environment, from proposed pigouvian taxes to mandatory labeling schemes to consumer education. When they work, which isn’t often, the effect is usually incredibly small.4 But by and large, this is because more heavy-handed regulation hasn’t been attempted in any way.
This is when everyone chimes in with their this doesn’t work, libertarian, Oreos have positive utility by making people happy, everyone needs to eat, what about food deserts counter-arguments. Almost everyone I know has thrown up their hands on regulating the food environment. We’re happy to hype GLP-1s because diet, education, exercise programs, etc. etc. didn’t work. Stephan Guyenet, pretty much the smartest person I know on this topic, is on the record saying to Ezra Klein that it’s hard not to see a technological solution to the obesity crisis. I agree.
But I still want to linger on that, because I think it suggests there is a range of problems — say total fertility rate — that are individual-level choices influenced by macro-level policy choices that are extremely hard to control. It should give us pause that we never figured out how to create a healthy food environment.
There is a pyrrhic nature to the success of GLP-1s. There is something unsettling in the fact that rather than regulate the food environment, the winning approach is for either individuals or governments to spend thousands of dollars a year on an injectable that affects changes in your brain.
Thomas Chatterton Williams got ratioed for this, probably more deservedly than not.5 “Deservedly” because we really don’t have good evidence of effective weight loss interventions, and his proposal changes little. But “not” because the idea that GLP-1s are suboptimal has weirdly, quickly, become controversial?
The degree to which this has become polarized is concerning. We’re in the weird timeline where both left and right have rejected policy-level solutions in favor of individual responsibility. In one you are responsible for finding and paying for a drug you will take once a week for the rest of your life. In the other, healthy food and exercise, and maybe no red dyes or corn syrup, I guess.
Lots of people are assholes on Twitter about this. We’ve already experienced enough polarization with obesity. I would so much prefer if GLP-1-stans approached this with civility rather than scorn, and stopped trying to shove progress-pills down everyone’s throats.
Trade-offs
And so mostly I’m asking for a little bit more humility.
These drugs seem really special. I spent seven years of my life in a PhD program looking at obesity trends and feeling deeply pessimistic about progress. That’s now changed.
But the same humility that makes us acknowledge these drugs' apparently magical effects should also make us watch carefully for delayed side effects or complications we haven't predicted. Real medicine usually involves tradeoffs - for GLP-1s to be truly different would be extraordinary. We have been here before. The entire reason that Medicare doesn’t cover obesity treatment is that historically, weight loss drugs that proved effective at reducing body mass also caused serious issues In the 1990s, Fen-phen was withdrawn after causing heart valve damage. Similarly, Meridia (sibutramine) was taken off the market in 2010 due to increased risk of cardiovascular events including strokes.
We have more long-term data on GLP-1s, and the data on long-term use suggests nothing on this scale is of concern. But there may be as yet unpredicted consequences. Maybe we'll find out that constantly signaling satiety has downsides we haven't discovered yet. Maybe real-world effectiveness diminishes compare to clinical trials. Or maybe we really have stumbled onto a biochemical lever that modern life pulled too far in one direction, and these drugs just push it back.
The next decade will tell us which story is right. But in the interim it’s worth remembering that we haven’t yet arrived — and won’t for many years — at obesity as a solved problem.
It might have fallen earlier, but NHANES, where the data comes from is intermittent. We won’t get the next data until 2026. It remains to be seen whether the trend continues. While we can’t for sure pinpoint drugs like Ozempic as the reason, the timing coincides with their rise, and the reversal trend is stronger among college-educated and therefore more likely to afford GLP-1s.
Bariatric surgery is the exception.
Other related compounds, such as tirzepatide (mounjaro) are even more effective. I’m not doing a full review here, and there’s likely other numbers that are more optimistic. Still, I expect as is generally the case, real-world effectiveness will be substantially lower than clinical efficacy.
Scott Kaplan has a great review on soda taxes in California vs. Big Soda.
I absolutely think there’s some weird truth in anti-GLP-1 discourse being related to the perceived status of being thin.











Genuine question: why would you expect at all that there *would* be a non-pharmacological solution to obesity? Given your PhD work I’m surprised that even due to the inefficacy of pretty much everything we are willing to try so far you still seem concerned that there’s a non-technological (“coordination”?) solution out there that would put a dent in obesity with anywhere near the same order of magnitude